In the multifaceted panorama of reproductive health, the phenomenon of disordered proliferative phase endometrium emerges as a significant yet often overlooked narrative. The cellular intricacies and physiological responses during the menstrual cycle exemplify a delicate interplay within the female body. The disordered proliferative phase is marked by aberrations in the endometrial lining, raising vital questions about menstrual health and fertility. This article aims to unpack the complexities of this condition and its implications in women’s health.
Understanding the Menstrual Cycle: A Harmonious Symphony
To fully appreciate the nuances of disordered proliferative phase endometrium, one must first contextualize it within the larger framework of the menstrual cycle. The menstrual cycle is a cyclical orchestration involving hormonal fluctuations that govern the development and shedding of the endometrial lining. This intricate process can be delineated into four key phases: the follicular phase, ovulation, the luteal phase, and menstruation.
During the follicular phase, estrogen levels rise, stimulating the proliferation of the endometrial tissue in preparation for potential implantation of a fertilized ovum. The ideal scenario is a precisely regulated proliferative phase, resulting in a uniformly thickened endometrial lining. However, disruptors such as hormonal imbalances, chronic stress, or environmental toxins can lead to disordered proliferation.
How Disordered Proliferative Phase Manifests
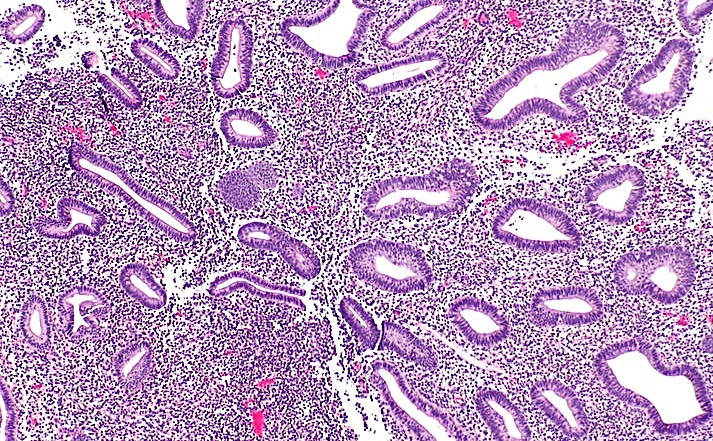
Disordered proliferative endometrium is typically characterized by abnormal endometrial growth patterns. Histologically, this condition may manifest as irregular glandular architecture, increased stromal cellularity, or a prominent presence of inflammatory cells. Such anomalies can lead to excessive thickening of the endometrial lining, medically termed endometrial hyperplasia.
The manifestations of a disordered proliferative phase may be insidious, often going unnoticed until they culminate in more pronounced symptoms. Menstrual irregularities, such as oligomenorrhea (infrequent menstruation) or amenorrhea (absence of menstruation), may be one of the first signs prompting further investigation. Additionally, women may experience menorrhagia, a condition marked by heavy or prolonged menstrual bleeding, often resulting in debilitating symptoms that interfere with daily life.
The Precipitating Factors: Unraveling the Causes
Embarking on an exploration of the etiology of disordered proliferative phase endometrium reveals a complex interplay of intrinsic and extrinsic factors. Hormonal dysregulation, notably an imbalance between estrogen and progesterone, is a primary contributor. Conditions such as polycystic ovary syndrome (PCOS) often lead to prolonged exposure to estrogen without the counterbalancing effect of progesterone, disrupting the normal cyclical pattern of endometrial proliferation.
Further complicating the clinical picture are genetic predispositions and lifestyle factors. Obesity, for instance, has a well-established link to increased estrogen levels through peripheral conversion of androgens. Inadequate physical activity, poor nutritional habits, and exposure to endocrine-disrupting chemicals can also exacerbate this hormone-driven cycle of misregulation.
Diagnostic Dilemmas: Navigating the Assessment Journey
Diagnosis of disordered proliferative phase endometrium typically involves a multi-pronged approach. A comprehensive medical history and physical examination provide crucial initial insights into the patient’s reproductive health status.
Transvaginal ultrasound is often employed as a non-invasive first-line imaging technique. The presence of an abnormally thickened endometrial stripe may prompt further investigation. However, the definitive diagnosis frequently necessitates a histopathological examination through endometrial biopsy. This procedure allows for direct assessment of cellular architecture, confirming the presence of disordered proliferation.
Challenges may arise in accurately diagnosing disordered proliferative endometrium. Clinicians may face the dilemma of distinguishing between physiological and pathological findings, particularly when dealing with atypical presentations. Thus, a multidisciplinary approach, involving gynecologists, endocrinologists, and pathologists, may provide a more holistic perspective on patient management.
Treatment Perspectives: A Tailored Approach
The treatment paradigm for disordered proliferative phase endometrium is invariably personalized, pivoting on the underlying cause and the patient’s reproductive aspirations. Hormonal therapy remains a cornerstone, particularly the administration of progestins to counteract the effects of unopposed estrogen. This therapeutic measure aims to normalize endometrial proliferation and mitigate the risk of endometrial hyperplasia.
For patients seeking to conceive, fertility treatments may be explored, particularly in the context of hormonal imbalances such as in PCOS. Clomiphene citrate, a widely recognized ovulatory stimulant, may facilitate regular ovulation, thereby enhancing the prospects of conception.
In more severe or refractory cases, surgical interventions such as dilation and curettage (D&C) may be necessary. This minimally invasive procedure not only provides paradoxical relief through the removal of excess endometrial tissue but also serves as a diagnostic tool for further histological evaluation.
The Implications of Disordered Proliferative Phase Endometrium
Examining disordered proliferative phase endometrium necessitates a broader dialogue about women’s health. The prevalence of this condition underscores the urgent need for greater awareness, early detection, and equitable access to healthcare resources. Often shrouded in stigma and misinformation, menstrual health remains a neglected area, with many women hesitant to voice their concerns.
By fostering open dialogues around menstrual irregularities and promoting education about reproductive health, society can dismantle taboos that inhibit women’s healthcare engagement. Empowering women with knowledge and resources facilitates advocacy not only for individual health but for systemic changes that prioritize women’s health in medical research and policy.
Conclusion: A Call to Reflection
In summation, the exploration of disordered proliferative phase endometrium reveals a tapestry woven from a variety of threads—hormonal dynamics, individual health profiles, and societal perceptions of women’s health. The challenge before us is to engage in a reflective inquiry into our understanding of reproductive health.
As individuals, scholars, and advocates, the journey does not end with the mere recognition of disordered proliferative phase endometrium. Instead, it beckons us to delve deeper into the underlying systems that perpetuate women’s health disparities. The dialogue surrounding these issues is critically important. How can we contribute to a more equitable healthcare landscape that addresses the unique needs of women? The answer lies in adopting an interdisciplinary approach—one that integrates scientific inquiry with passionate advocacy for reproductive justice.