Alcohol consumption has long been a focal point of public health discussions, particularly regarding its implications for cardiovascular health. The ubiquitous presence of alcohol in social and cultural practices often obscures the increasingly complex relationship between its consumption and the prevalence of cardiovascular disease (CVD). This article seeks to elucidate the multifaceted interplay between alcohol intake and cardiovascular health, outlining the risks and, in some contexts, the perceived benefits associated with varying levels of consumption.
The Cardiovascular System: A Primer
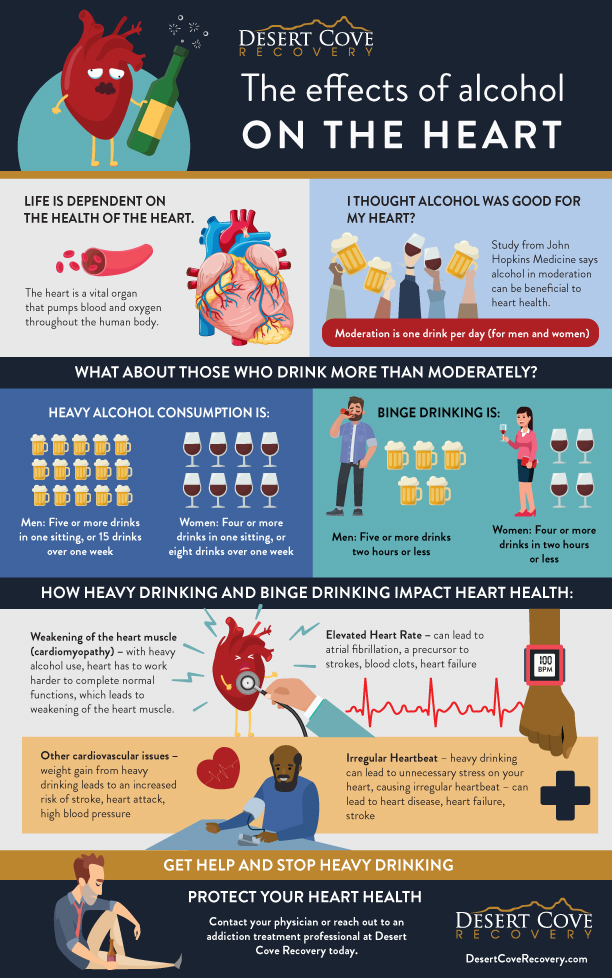
Understanding the cardiovascular system is essential for appreciating how alcohol affects heart health. The cardiovascular system comprises the heart, blood vessels, and blood, working in concert to deliver oxygen and nutrients to tissues while facilitating the removal of waste products. Cardiovascular disease encompasses a range of disorders, including coronary artery disease, hypertension, stroke, and heart failure, all of which are influenced by a myriad of genetic, environmental, and lifestyle factors, including diet and alcohol consumption.
The Dichotomy of Alcohol’s Effects
Alcohol, particularly ethanol, has a dualistic reputation in medical literature. On one hand, moderate consumption has been purported to offer some cardioprotective effects, leading to the suggestion that red wine, with its polyphenolic compounds, may reduce the risk of coronary heart disease. This phenomenon is often attributed to the increase in high-density lipoprotein (HDL) cholesterol and improved endothelial function, which facilitates vasodilation and reduces arterial stiffness.
However, the notion of “moderate” consumption is highly nuanced and varies significantly among individuals. The threshold is often defined as one drink per day for women and two for men. Epidemiological studies suggest that exceeding these limits can lead to a plethora of cardiovascular complications, including increased systolic blood pressure, dyslipidemia, and the exacerbation of arrhythmias. Furthermore, the relationship between alcohol and cardiovascular health is dose-dependent; even modest elevations in intake can have cumulative detrimental effects over time.
Alcohol and Hypertension: A Close Connection
One of the most salient associations between alcohol consumption and cardiovascular disease lies in the influence of alcohol on blood pressure. Hypertension, or high blood pressure, directly increases the risk for heart disease and stroke. Evidence shows that alcohol acts as a pressor agent, inducing vasoconstriction and activating the sympathetic nervous system. Chronic alcohol consumption has been linked to elevated blood pressure levels, thereby increasing the risk of hypertensive heart disease.
Moreover, the acute effects of excess alcohol consumption, often resulting in binge drinking, can induce significant spikes in blood pressure. These transient but dramatic fluctuations may cause immediate harm to cardiovascular structures, leading to endothelial dysfunction. Studies have indicated a bidirectional relationship, where individuals with pre-existing hypertension may consume alcohol as a coping mechanism, further exacerbating their condition.
Alcohol and Atrial Fibrillation: The Arrhythmia Connection
Atrial fibrillation (AF), a common form of arrhythmia, is another concern linked to alcohol intake. AF is characterized by disorganized electrical activity in the atria, leading to a rapid and irregular heartbeat. Research has demonstrated that heavy alcohol consumption can precipitate AF episodes, a phenomenon sometimes referred to as “holiday heart syndrome.” This condition often manifests after periods of binge drinking, contributing to increased morbidity and hospitalizations.
Interestingly, some studies have indicated that light to moderate alcohol consumption is not necessarily a predictor for AF, yet this does not negate the potential risks associated with excessive intake. In fact, the American College of Cardiology emphasizes that the detrimental effects of high alcohol consumption on heart rhythm and rate should not be overlooked, serving as a reminder that the line between moderate enjoyment and harmful overconsumption is perilously thin.
Coronary Artery Disease: A Delicate Balance
The relationship between alcohol and coronary artery disease (CAD) underscores the precarious balance of benefits and risks inherent in alcohol consumption. On one side, moderate alcohol intake has been demonstrated to correlate with a reduced risk of CAD, potentially due to improved lipid profiles and anti-inflammatory effects. Furthermore, certain components found in beverages, such as resveratrol in red wine, might confer additional cardioprotective properties.
Conversely, heavy drinking is a well-established risk factor for CAD. It induces adverse changes in lipid metabolism, elevates triglyceride levels, and accelerates atherosclerotic processes. The chronic inflammatory response incited by excessive alcohol consumption can lead to plaque formation, resulting in obstruction of coronary arteries and subsequent myocardial ischemia. Thus, individuals who indulge in heavy drinking are often at an elevated risk of acute coronary syndromes, including myocardial infarctions.
Long-Term Consequences of Alcohol Abuse
Alcohol abuse is not a harmless endeavor; it results in a cascade of biological, psychological, and social consequences. The direct impact on cardiovascular health is compounded by associated factors such as lifestyle choices, nutritional deficiencies, and comorbid conditions. Individuals with chronic alcohol use disorders frequently present with anemia, electrolyte imbalances, and malnutrition, all of which can adversely affect heart function.
Additionally, the interplay between alcohol consumption and mental health is significant; anxiety and depression can lead to increased alcohol consumption as a form of self-medication. This creates a vicious cycle where both alcohol abuse and cardiovascular diseases perpetuate one another, ultimately compromising overall health and wellbeing.
Preventive Strategies and Public Health Considerations
Understanding the conundrum of alcohol consumption necessitates precise public health strategies that address consumption patterns while promoting education about its risks. Recommendations should be tailored to the individual, taking into account personal and familial risk factors for cardiovascular disease. Accessible support programs for those struggling with alcohol use disorder, alongside initiatives to encourage moderation, can play a critical role in mitigating the adverse cardiovascular effects of alcohol.
Moreover, healthcare providers should engage in meaningful conversations about alcohol consumption with their patients, emphasizing the importance of making informed choices. Comprehensive health education, including the risks associated with binge drinking and the benefits of moderation, can empower individuals to make healthier lifestyle decisions.
Conclusion: Navigating the Terrain of Alcohol and Heart Health
The intersection of alcohol consumption and cardiovascular disease is a multifaceted issue that requires a nuanced understanding of both risks and potential benefits. While light to moderate consumption may present some cardioprotective factors, the dangers of excess consumption cannot be overstated. A conscientious approach to alcohol intake, guided by informed choices and support systems, becomes crucial in the quest to maintain cardiovascular health. Ultimately, the journey toward understanding and managing alcohol’s impact on heart health is ongoing, requiring dedicated research, public health initiatives, and personal vigilance.