The intricate tapestry of the female reproductive system is woven with myriad complexities, among which disordered proliferative endometrium stands out as a significant histological phenomenon. This condition, characterized by atypical glandular developments and an aberrant architecture of the endometrial lining, garners attention not only due to its pathological implications but also for its profound association with various reproductive health outcomes.
Understanding disordered proliferative endometrium necessitates an exploration of the normal histological features of the endometrium. The endometrium undergoes cyclical changes throughout the menstrual cycle, commencing with the proliferative phase which is stimulated primarily by estrogen. Within this phase, the endometrial lining thickens, with the proliferation of both stromal and glandular components. The hallmark features include well-organized glands, abundant blood vessels, and a cohesive stroma that collectively prepare the uterus for potential implantation.
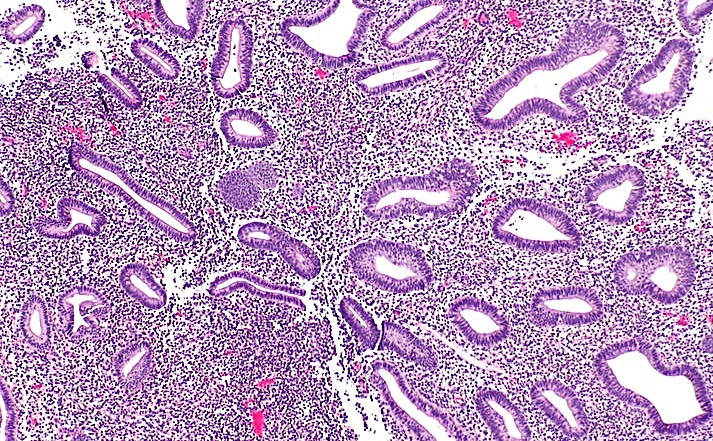
However, deviations from this normative state manifest as disordered proliferative endometrium. This disorder often arises due to hormonal imbalances, particularly involving estrogen and progesterone. The disordered histological appearance typically entails irregularities in gland formation—such as cystic dilatation, increased gland density, or a heterogeneity in the size and shape of the glands—coupled with a disorganized stromal framework. This pathological condition may signal the presence of various underlying endocrine disorders, and possibly, a prelude to hyperplasia or even malignancy.
In delving into the histological characteristics, one notes that the glandular structures become misaligned and undergo an aberrant pattern of growth. The proliferation of endometrial cells tends to exceed the typical limits, leading to a hyperplastic, yet atypical appearance that challenges diagnostic clarity.
Evaluating the clinical implications of disordered proliferative endometrium is crucial. Evidence suggests that individuals with this condition may experience an array of clinical manifestations, which can have cascading effects on both mental and physical well-being.
The interplay between reproductive health and psychological resilience cannot be overstated. The prospect of dealing with a disordered proliferative endometrium may evoke feelings of anxiety, frustration, and uncertainty regarding reproductive futures. As women navigate their reproductive choices and face potential health concerns, the fundamental connection between physical and mental health becomes paramount, highlighting the necessity of a support system that fosters mood enhancement and emotional well-being.
Moreover, it should be noted that the management of disordered proliferative endometrium typically emphasizes hormonal regulation. Treatment modalities often focus on restoring hormonal balance through progestogens or intrauterine devices (IUDs) that release hormones. These interventions have been shown to ameliorate symptoms, regulate menstrual cycles, and enhance overall quality of life for affected individuals.
The diagnostic process is multifaceted, often incorporating imaging techniques such as ultrasound and histopathological assessments via endometrial biopsy. These methodologies not only facilitate the confirmation of disordered proliferative endometrium but also serve as a vital component of the comprehensive evaluation of reproductive health.
The mood-boosting experiences associated with properly addressing disordered proliferative endometrium cannot be overlooked. Empowerment through knowledge is essential; individuals engaging with their healthcare providers about the implications of their diagnosis often report a sense of agency that is vital for emotional stability. Through education, women can demystify the pathophysiological aspects of their condition, transforming apprehension into understanding.
Providing a safe space for open conversations regarding reproductive health fosters a supportive environment where emotions can be freely expressed. This social support can profoundly uplift mood and enhance resilience, establishing a network of understanding that champions women’s health.
Furthermore, the psychological ramifications of disordered proliferative endometrium may be alleviated through lifestyle modifications. Encouraging women to adopt holistic health practices, such as exercise, mindful eating, and stress reduction techniques, can contribute positively to both physical and mental health, thus fostering an overall enhancement in mood.
The interplay between mental health and physical health is reinforced through individual accounts revealing significant improvements in emotional well-being following intervention for disordered proliferative endometrium. Whether it’s the relief of pain, regulation of menstrual cycles, or the waning of anxiety regarding fertility issues, the positive ramifications are profound.
Lastly, exploring community-based interventions and support groups can yield significant benefits. Participatory groups allow women to share experiences, thereby generating collective resilience that fortifies mental health. By finding common ground and shared narratives, women cultivate solidarity and empowerment, fostering an atmosphere of support that transcends individual diagnoses.
In conclusion, the examination of disordered proliferative endometrium histology reveals not only the intricate biological mechanisms underlying this condition but also emphasizes the importance of holistic approaches to health management. By addressing both the physical and psychological dimensions of reproductive health, one can cultivate a mood-boosting experience that empowers women to embrace their health journeys with optimism and strength.