Neurofeedback therapy, an innovative intervention rooted in principles of biofeedback and neurophysiological regulation, has emerged as a focal point in contemporary psychological and psychiatric discourse. As practitioners and researchers alike delve deeper into the intricacies of human cognition and emotional health, questions regarding its effectiveness proliferate, igniting conversations around its potential to revolutionize treatment modalities for various psychological disorders.
The allure of neurofeedback lies in its promise of an interactive, non-invasive approach to treating conditions such as anxiety, depression, ADHD, and PTSD. Unlike traditional therapeutic methods, which often emphasize verbal exchanges and cognitive restructuring, neurofeedback directly engages with the neural frameworks that underpin behavior and emotional regulation. Consequently, an exploration into the efficacy of this technique reveals a burgeoning field rife with both potential and controversy.
In this discourse, we shall unravel the multifaceted dimensions of neurofeedback therapy, articulating not only its foundational mechanisms and applications but also providing insights into its empirical validation within therapeutic contexts.
Essential Mechanisms Underpinning Neurofeedback Therapy
At its core, neurofeedback therapy seeks to enhance self-regulation of brain activity. Through real-time feedback, individuals gain insights into their brainwave patterns via EEG technology. This feedback loop assists users in recognizing specific mental states and employs operant conditioning to reinforce desirable brain states associated with calmness, focus, or emotional stability.
The predominant modalities of neurofeedback are categorized into two broad avenues: frequency training and amplitude training. In frequency training, specific brainwave frequencies, such as beta waves associated with alertness or alpha waves tied to relaxation, are targeted for modification. Conversely, amplitude training seeks to enhance or suppress the strength of specific frequency bands, allowing for adaptive changes in neural functioning.
Neurofeedback’s emphasis on neuroplasticity—a term denoting the brain’s ability to reorganize itself by forming new neural connections throughout life—underscores its theoretical appeal. This capacity for adaptation invites intrigue into the brain’s potential for transformation, promising not only symptom alleviation but also psychological growth and resilience in individuals grappling with various mental health challenges.
Applications of Neurofeedback Therapy: A Spectrum of Disorders
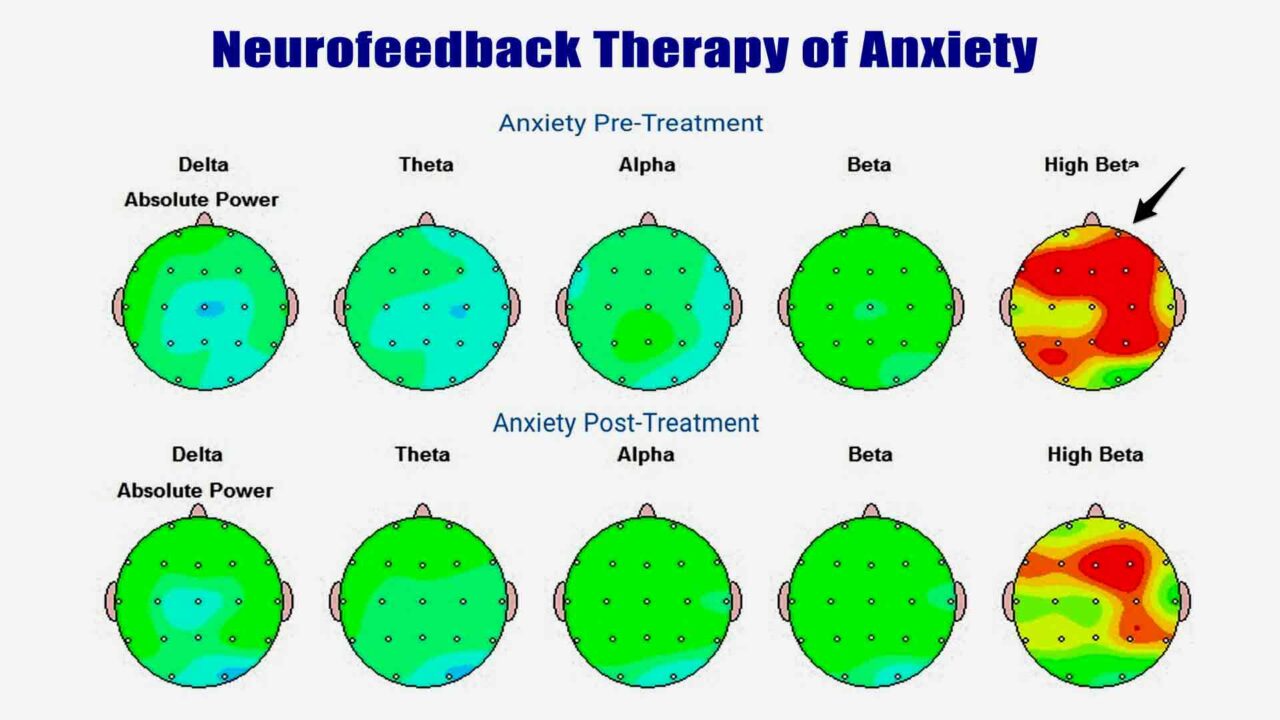
The clinical applications of neurofeedback therapy are diverse, spanning numerous psychological disorders. Among the most compelling areas of exploration is its use in treating anxiety disorders, where the ability to modulate hyperactive brain regions implicated in fear responses may result in significant symptom relief.
One notable study found that participants with anxiety reported substantial reductions in symptoms following a series of neurofeedback sessions aimed at cultivating alpha wave production. Such findings suggest that neurofeedback can promote a state of calmness and reduce reactivity to stress-inducing stimuli. Similarly, applications in managing ADHD behaviors have garnered attention, as neurofeedback may enhance attentional control through targeted modulation of theta and beta wave activity.
Furthermore, the efficacy of neurofeedback therapy extends beyond anxiety and ADHD; its incorporation into trauma-informed practices for PTSD illustrates its versatility. Research indicates that neurofeedback may assist individuals in reprocessing trauma-related memories and in mitigating the hyperarousal typically associated with this condition.
While anecdotal evidence and clinical experiences abound, the overarching question relies on whether such outcomes stand the scrutiny of dual quantitative and qualitative analysis. Can the neurofeedback industry, often viewed with skepticism, offer empirical results that elevate its status within accepted clinical frameworks?
Empirical Validation and Controversies Surrounding Efficacy
Despite the promising anecdotes and preliminary studies, the empirical validation of neurofeedback therapy remains contentious. Many critics argue that the current body of literature, while indeed burgeoning, is fraught with methodological limitations. Small sample sizes, lack of control groups, and biases stemming from practitioners with vested interests often cloud the clarity around neurofeedback’s effectiveness.
However, emerging meta-analyses present a more nuanced understanding, highlighting that, when proper experimental designs are employed, neurofeedback demonstrates positive effects across various populations. An analysis encompassing multiple randomized controlled trials revealed statistically significant improvements in symptom severity for anxiety and ADHD through neurofeedback interventions compared to control conditions.
Moreover, the placebo effect—maligned in the annals of rigorous scientific inquiry—cannot be wholly dismissed; the subjective experience of undergoing neurofeedback may yield intrinsic benefits irrespective of the act itself. As subjects report feelings of empowerment and self-awareness post-treatment, the significance of components beyond mere neurological data emerges.
Navigating the Future of Neurofeedback Therapy
In light of the current scrutinies and accolades, the future of neurofeedback therapy holds tantalizing potential. Methodological advancements combined with interdisciplinary collaboration could yield groundbreaking innovations, increasing the reliability and applicability of neurofeedback across broader demographics and conditions.
Moreover, the impending integrations of artificial intelligence and machine learning algorithms could enhance the precision of neurofeedback training, unlocking paradigms of personalized treatment that were previously unimaginable. Such technological advancements not only foster an environment ripe for refined therapeutic techniques but also entice dialogues around ethical considerations, accessibility, and the commercialization of mental health interventions.
In synthesizing these findings, it is pertinent to catalyze an ongoing dialogue regarding the promises and perils surrounding neurofeedback therapy. Advocates extol its virtues and potential transformative impact on mental healthcare, whereas critics express warranted caution against overreliance on insufficiently standardised procedures. Engaging in a multidisciplinary conversation invites diverse perspectives and fosters a critical examination of neurofeedback’s role within an evolving therapeutic landscape.
Conclusively, while neurofeedback’s efficacy may fluctuate amidst proliferating opinions and emerging data, its unique capacity to explicate the bridges between neuroscience and impactful therapy is irrefutable. As we navigate the complexities of mental health treatments, the promise of a shift in perspective offered by neurofeedback beckons further research and contemplation. Such inquiries not only pique curiosity but urge a broader understanding of human cognitive experience and the limitless potential for healing.